Transient Ischemic Attack: Symptoms, Causes, Treatment
What are the symptoms of a transient ischemic attack?
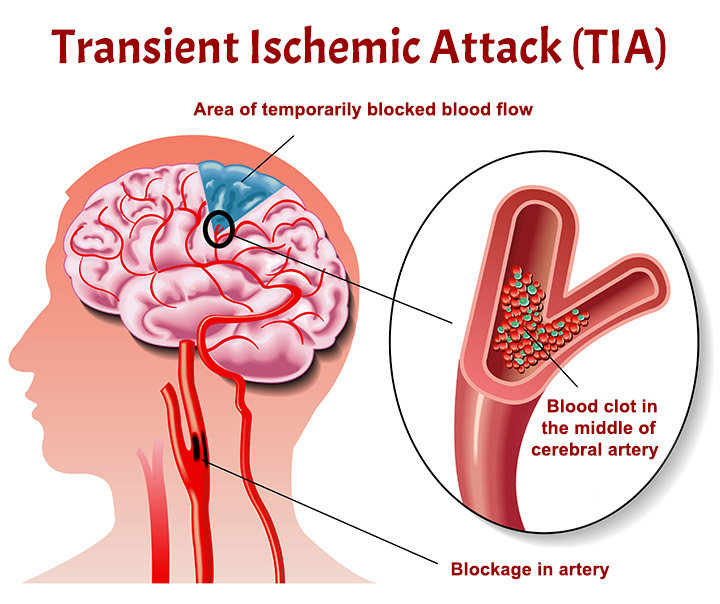
A transient ischemic attack (TIA), often referred to as a “mini-stroke,” is a temporary disruption of blood flow to the brain, usually caused by a blood clot. The symptoms of a TIA are similar to those of a stroke but typically last for a shorter period of time (usually a few minutes to a few hours) and do not cause permanent brain damage. However, a TIA is a warning sign that a more serious stroke may occur in the future and should be taken seriously.
The symptoms of a TIA can vary depending on the area of the brain affected, but may include:
- Sudden weakness or numbness in the face, arm, or leg, especially on one side of the body.
- Sudden difficulty speaking or understanding speech.
- Sudden vision changes in one or both eyes, such as double vision or loss of vision.
- Sudden dizziness, loss of balance, or coordination.
- Sudden severe headache with no known cause.
It’s important to seek immediate medical attention if you experience any of these symptoms, even if they go away quickly. TIAs are often a warning sign that a more severe stroke may occur in the future, and prompt treatment can help reduce the risk of a stroke. Treatment for a TIA may include medications to prevent blood clots, reduce blood pressure, or lower cholesterol levels, as well as lifestyle changes to reduce the risk of future TIAs or strokes.
What are the causes of a transient ischemic attack?
A transient ischemic attack (TIA) is caused by a temporary disruption of blood flow to the brain, usually due to a blood clot or other blockage in an artery that supplies blood to the brain. The blockage can be caused by a variety of factors, including:
- Atherosclerosis: Atherosclerosis is a condition in which the arteries become narrowed and hardened due to the buildup of plaque (a combination of cholesterol, fats, and other substances). Plaque buildup can restrict blood flow and increase the risk of blood clots, which can lead to a TIA.
- Blood clots: Blood clots can form in the arteries that supply blood to the brain or can travel from other parts of the body (such as the heart) to the brain, causing a blockage and a TIA.
- Atrial fibrillation: Atrial fibrillation is an irregular heart rhythm that can cause blood to pool in the heart, increasing the risk of blood clots. If a blood clot forms in the heart and travels to the brain, it can cause a TIA.
- Carotid artery disease: Carotid artery disease occurs when the carotid arteries, which supply blood to the brain, become narrowed or blocked due to atherosclerosis or other factors. This can increase the risk of blood clots and TIAs.
- Other heart conditions: Certain heart conditions, such as heart valve abnormalities or a history of heart attack, can increase the risk of blood clots forming and causing a TIA.
- Smoking: Smoking damages the blood vessels and increases the risk of atherosclerosis and blood clots, which can lead to a TIA.
- High blood pressure: High blood pressure can damage the blood vessels and increase the risk of atherosclerosis and blood clots, increasing the risk of a TIA.
- High cholesterol: High levels of cholesterol in the blood can lead to atherosclerosis and increase the risk of a TIA.
- Diabetes: Diabetes can damage the blood vessels and increase the risk of atherosclerosis and blood clots, increasing the risk of a TIA.
- Obesity: Obesity is a risk factor for atherosclerosis, high blood pressure, and diabetes, all of which can increase the risk of a TIA.
- Family history: A family history of stroke or TIA can increase the risk of experiencing a TIA.
It’s important to note that not all TIAs have a clear cause, and some may occur without any obvious underlying condition. However, addressing and managing the risk factors mentioned above can help reduce the risk of experiencing a TIA.
What is the treatment for a transient ischemic attack?
The treatment for a transient ischemic attack (TIA) aims to reduce the risk of a future stroke by addressing the underlying causes and risk factors. Treatment may include:
- Medications:
- Antiplatelet drugs, such as aspirin or clopidogrel, may be prescribed to reduce the risk of blood clot formation.
- Anticoagulant drugs, such as warfarin or direct oral anticoagulants (DOACs), may be used if the TIA is caused by atrial fibrillation or another condition that increases the risk of blood clots.
- Blood pressure-lowering medications may be prescribed if high blood pressure is a contributing factor.
- Cholesterol-lowering medications, such as statins, may be prescribed to lower cholesterol levels and reduce the risk of atherosclerosis.
- Lifestyle changes:
- Adopting a healthy diet low in saturated fats, cholesterol, and salt, and rich in fruits, vegetables, and whole grains can help reduce the risk of atherosclerosis and stroke.
- Regular exercise can help improve cardiovascular health and reduce the risk of stroke.
- Quitting smoking and limiting alcohol consumption can also reduce the risk of stroke.
- Surgery or procedures:
- In some cases, surgery or procedures may be recommended to reduce the risk of stroke. For example, carotid endarterectomy may be performed to remove plaque buildup from the carotid arteries, or carotid angioplasty and stenting may be performed to open narrowed arteries.
- Education and support:
- Education about the risk factors for stroke and how to manage them can help reduce the risk of future TIAs or strokes.
- Support from healthcare providers, family, and friends can also be important in making lifestyle changes and adhering to treatment plans.
It’s important for individuals who have experienced a TIA to follow up with their healthcare provider regularly to monitor their condition and make any necessary adjustments to their treatment plan. Prompt treatment and lifestyle changes can help reduce the risk of future TIAs or strokes and improve overall cardiovascular health.