Ulcerative Colitis: Symptoms, Causes, Treatment
What are the symptoms of ulcerative colitis?
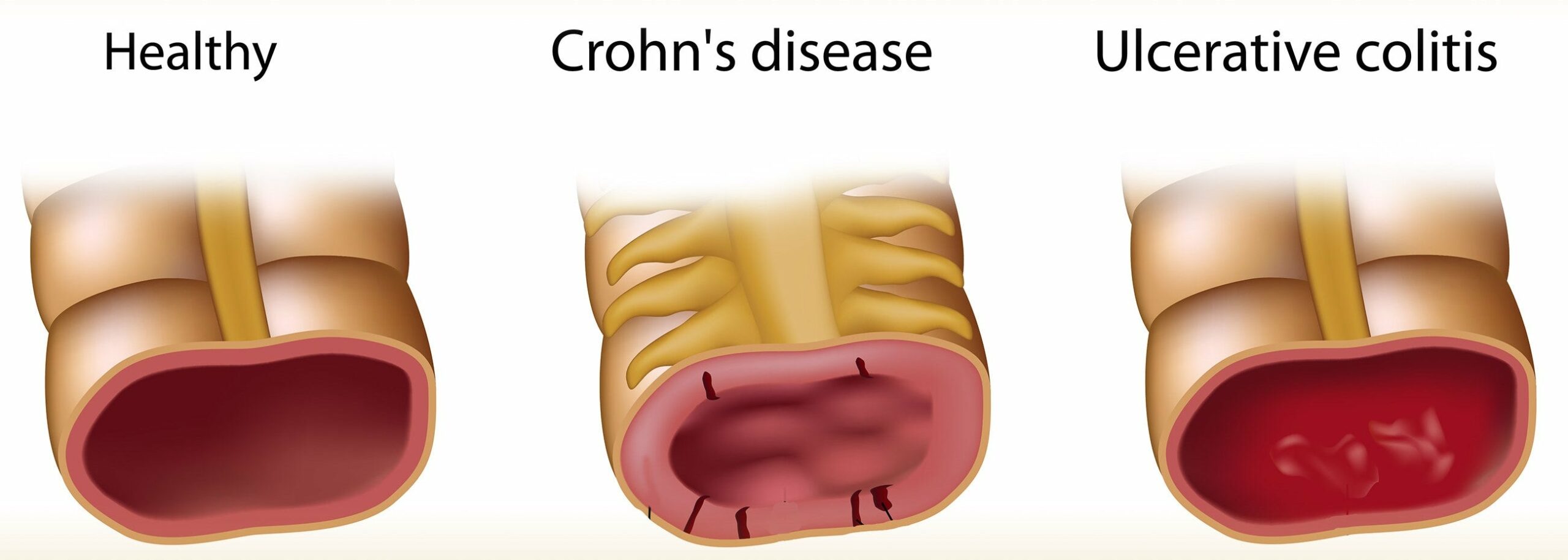
Ulcerative colitis (UC) is a chronic inflammatory bowel disease that causes inflammation and ulcers in the lining of the colon, also known as the large intestine. The symptoms of UC can vary from person to person, but common symptoms include:
- Diarrhea: Frequent and loose stools, often with blood or pus
- Abdominal pain: Cramping, discomfort, or tenderness in the abdomen, which can be relieved by bowel movements
- Rectal bleeding: Blood in the stool, which can be bright red or dark
- Tenesmus: A feeling of urgency or pressure to have a bowel movement, even if the bowels are empty
- Abdominal cramping: Painful cramping in the abdomen, which can be relieved by bowel movements
- Weight loss: Loss of weight due to malabsorption of nutrients and frequent diarrhea
- Fatigue: Feeling tired and weak due to chronic inflammation and malabsorption
- Loss of appetite: Decreased appetite due to nausea, abdominal pain, and discomfort
- Nausea and vomiting: Feeling sick to the stomach and vomiting due to inflammation and malabsorption
- Abdominal distension: Swelling or bloating of the abdomen due to gas and fluid accumulation
- Fatty or oily stools: Stools that are pale, greasy, or frothy due to malabsorption of fats
- Changes in bowel habits: Changes in bowel frequency, consistency, or stool shape
In addition to these symptoms, some people with UC may experience:
- Rectal fissures (tears) or anal fissures
- Hemorrhoids (swollen veins)
- Skin rashes or lesions
- Joint pain or arthritis
- Eye problems (such as conjunctivitis or uveitis)
- Mouth sores (aphthous ulcers)
- Hair loss
It’s important to note that UC symptoms can vary in severity and frequency, and some people may experience a mild form of the disease while others may have a more severe form that requires hospitalization. If you are experiencing symptoms of UC, it’s essential to consult with a healthcare provider for proper diagnosis and treatment.
What are the causes of ulcerative colitis?
The exact causes of ulcerative colitis (UC) are not yet fully understood, but it is believed to be a complex interplay of genetic, environmental, and immune system factors. Some of the potential causes of UC include:
- Genetic predisposition: UC is more common in people with a family history of the disease, and certain genetic mutations may increase the risk of developing UC.
- Environmental factors: Exposure to certain environmental triggers, such as smoking, stress, and certain foods, may contribute to the development of UC.
- Immune system dysfunction: The immune system is designed to protect the body from infection and disease, but in people with UC, the immune system can become overactive and mistakenly attack the lining of the colon, leading to inflammation and damage.
- Gut microbiome: The gut microbiome refers to the trillions of microorganisms that live in the gut and play a crucial role in our overall health. Research suggests that an imbalance of the gut microbiome, known as dysbiosis, may contribute to the development of UC.
- Leaky gut syndrome: Leaky gut syndrome is a condition where the lining of the gut becomes damaged, allowing toxins and undigested food particles to pass through the gut wall and into the bloodstream, triggering an immune response.
- Barrier dysfunction: The gut lining is designed to act as a barrier between the internal environment and the external environment. In people with UC, the barrier function may be disrupted, allowing toxins and other substances to pass through the lining and trigger inflammation.
- Inflammation: Chronic inflammation is a hallmark of UC, and it is thought to be driven by a combination of genetic, environmental, and immune system factors.
- Oxidative stress: Oxidative stress occurs when there is an imbalance between the production of free radicals (highly reactive molecules that can damage cells) and the body’s ability to neutralize them. This can lead to inflammation and tissue damage.
- Hormonal factors: Hormonal changes, such as those experienced during pregnancy or menstruation, may trigger UC symptoms in some people.
- Other factors: Other factors that may contribute to the development of UC include:
- Smoking
- Stress
- Certain medications
- Food sensitivities or intolerances
- Vitamin D deficiency
- Obesity
It’s important to note that UC is a complex condition, and it is likely that multiple factors contribute to its development. If you are experiencing symptoms of UC, it’s essential to consult with a healthcare provider for proper diagnosis and treatment.
What is the treatment for ulcerative colitis?
Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that causes inflammation and ulcers in the lining of the colon and rectum. The goal of treatment for UC is to reduce inflammation, control symptoms, and improve quality of life. Treatment for UC may include:
- Medications: Various medications are used to treat UC, including:
- Aminosalicylates (5-ASA): These medications reduce inflammation in the colon and are often used as first-line treatment for mild to moderate UC.
- Corticosteroids: These medications help reduce inflammation and are used to treat moderate to severe UC. They are typically used for short periods due to their potential side effects.
- Immunomodulators: These medications suppress the immune system and are used to treat moderate to severe UC that does not respond to other treatments.
- Biologic therapies: These medications target specific proteins in the immune system and are used to treat moderate to severe UC that does not respond to other treatments.
- Dietary changes: Some people with UC find that certain foods can trigger symptoms. Making dietary changes, such as avoiding dairy products or high-fiber foods, may help reduce symptoms.
- Lifestyle modifications: Stress can worsen symptoms of UC. Managing stress through techniques such as relaxation exercises, meditation, or counseling may help improve symptoms.
- Surgery: In severe cases of UC that do not respond to other treatments, surgery to remove the colon and rectum (proctocolectomy) may be necessary. This surgery cures UC but requires the use of a pouch or stoma to collect waste.
- Monitoring and follow-up: Regular monitoring by a healthcare provider is important to assess disease activity, monitor for complications, and adjust treatment as needed.
It’s important for individuals with UC to work closely with a healthcare provider to develop a treatment plan that is tailored to their specific needs. Treatment for UC is typically long-term and may require adjustments over time based on the individual’s response to treatment.