Urinary Incontinence in Women: Symptoms, Causes, Treatment
What are the symptoms of urinary incontinence in women?
Urinary incontinence in women is the unintentional loss of urine. The symptoms can vary depending on the type of incontinence, but common symptoms include:
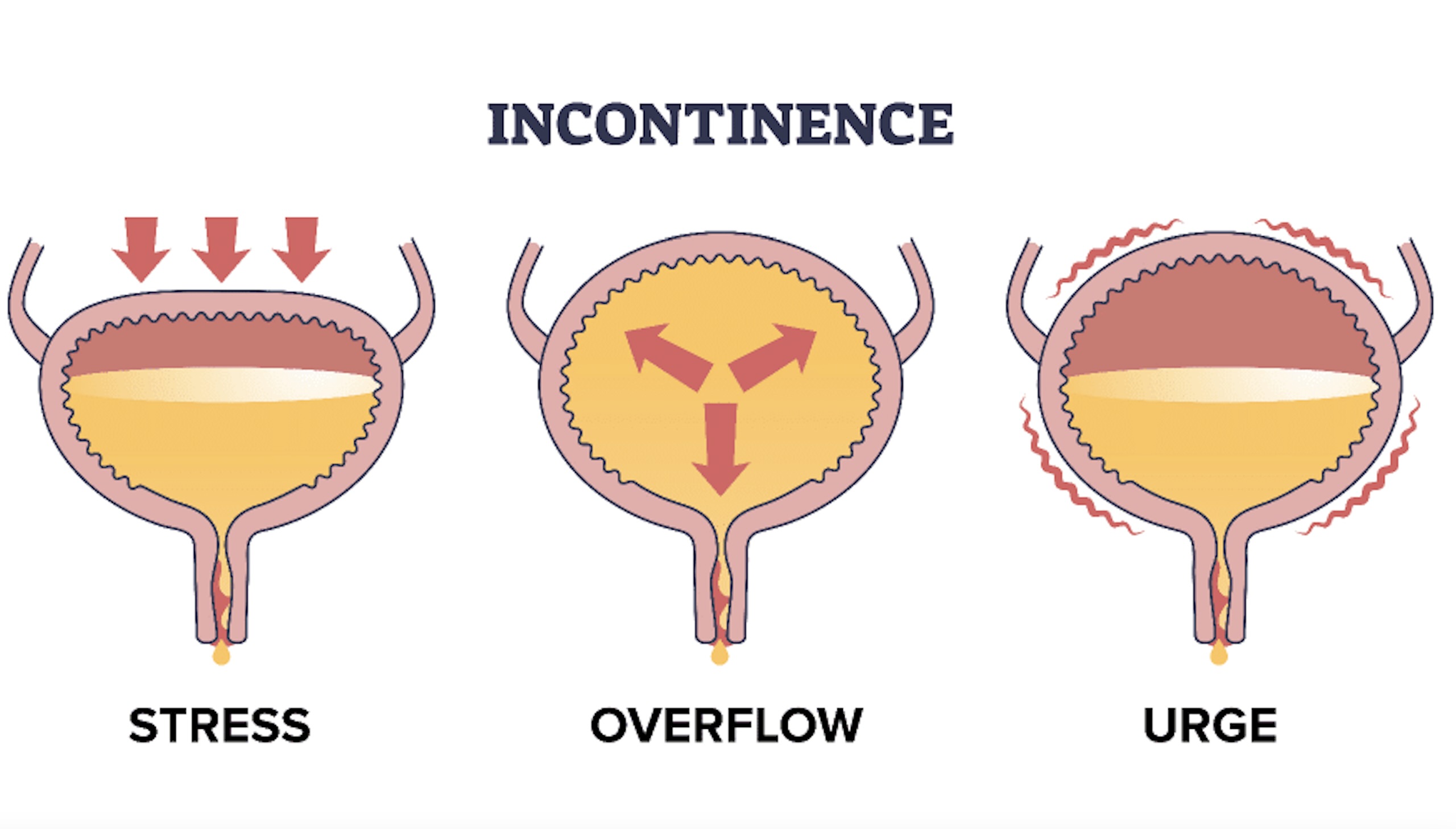
- Stress incontinence: Urine leakage that occurs when there is pressure on the bladder, such as during coughing, sneezing, laughing, or exercising.
- Urge incontinence: Sudden, intense urge to urinate followed by an involuntary loss of urine. People with urge incontinence may also need to urinate frequently, including waking up multiple times at night to urinate (nocturia).
- Overflow incontinence: Frequent or constant dribbling of urine due to an inability to completely empty the bladder.
- Mixed incontinence: A combination of stress and urge incontinence, where symptoms of both types are present.
- Functional incontinence: Difficulty reaching the toilet in time due to physical or cognitive impairment, even though the bladder may be functioning normally.
- Total incontinence: Continuous, unpredictable leakage of urine.
In addition to these symptoms, some women may also experience feelings of embarrassment, frustration, or a negative impact on their quality of life due to urinary incontinence. If you are experiencing symptoms of urinary incontinence, it’s important to talk to your healthcare provider for proper diagnosis and treatment.
What are the causes of urinary incontinence in women?
Urinary incontinence in women can be caused by various factors, including:
- Weak pelvic floor muscles: The muscles that support the bladder and urethra can weaken due to aging, childbirth, or other factors, leading to urinary incontinence.
- Pregnancy and childbirth: The pelvic floor muscles and nerves can be stretched and damaged during pregnancy and childbirth, increasing the risk of urinary incontinence.
- Menopause: Changes in hormone levels during menopause can lead to changes in the urinary tract and pelvic floor muscles, increasing the risk of urinary incontinence.
- Aging: As women age, the bladder and urethra can become less elastic, and the muscles that control urination can weaken, increasing the risk of urinary incontinence.
- Obesity: Excess weight can put pressure on the bladder and pelvic floor muscles, increasing the risk of urinary incontinence.
- Neurological disorders: Conditions such as stroke, multiple sclerosis, Parkinson’s disease, and spinal cord injuries can affect the nerves that control bladder function, leading to urinary incontinence.
- Urinary tract infections (UTIs): Infections in the urinary tract can irritate the bladder and urethra, leading to urinary incontinence.
- Medications: Some medications, such as diuretics, sedatives, and muscle relaxants, can increase the risk of urinary incontinence.
- Chronic coughing or constipation: Conditions that cause chronic coughing or straining can put pressure on the bladder and pelvic floor muscles, increasing the risk of urinary incontinence.
- Smoking: Smoking can irritate the bladder and increase the risk of urinary incontinence.
It’s important to note that urinary incontinence can have multiple causes, and the underlying cause may vary from person to person. If you are experiencing urinary incontinence, it’s important to talk to your healthcare provider for proper diagnosis and treatment.
What is the treatment for urinary incontinence in women?
The treatment for urinary incontinence in women depends on the type and severity of the condition. Treatment options may include:
- Lifestyle changes: Making changes to your lifestyle can help manage urinary incontinence. This may include losing weight, avoiding caffeine and alcohol, quitting smoking, and practicing bladder training exercises to improve bladder control.
- Pelvic floor muscle exercises (Kegel exercises): Strengthening the pelvic floor muscles can help improve bladder control and reduce urinary incontinence. A physical therapist or healthcare provider can provide guidance on how to perform these exercises correctly.
- Bladder training: Bladder training involves gradually increasing the time between bathroom visits to help improve bladder control. This can help train the bladder to hold urine for longer periods.
- Medications: Your healthcare provider may prescribe medications to help relax the bladder muscles or reduce bladder contractions, depending on the type of urinary incontinence you have.
- Devices: Devices such as pessaries or urethral inserts can help support the bladder and reduce urinary incontinence.
- Medical devices: For some types of urinary incontinence, medical devices such as a urethral sling or artificial urinary sphincter may be recommended to help control urine flow.
- Surgery: In some cases, surgery may be recommended to correct anatomical issues that contribute to urinary incontinence, such as a prolapsed bladder or urethra.
- Behavioral therapies: Behavioral therapies, such as biofeedback or electrical stimulation, can help improve bladder control and reduce urinary incontinence.
- Injections: Injections of bulking agents into the tissues around the urethra can help reduce urinary incontinence by providing support to the urethra.
The most appropriate treatment for urinary incontinence will depend on the underlying cause and the severity of the condition. It’s important to talk to your healthcare provider for a proper evaluation and to discuss the best treatment options for you.