Vaginal Cancer: Symptoms, Causes, Treatment
What are the symptoms of vaginal cancer?
Vaginal cancer is a rare type of cancer, and its symptoms can be easily overlooked or mistaken for other conditions. Here are some common symptoms of vaginal cancer:
- Abnormal vaginal bleeding: This is the most common symptom of vaginal cancer. It can occur between periods, after menopause, or after intercourse.
- Abnormal vaginal discharge: The discharge may be watery, foul-smelling, or contain blood.
- Pelvic pain: Women with vaginal cancer may experience pelvic pain or pressure, especially during intercourse or urination.
- Difficult or painful urination: The cancer can sometimes affect the bladder or urethra, leading to discomfort during urination.
- Constipation or difficult bowel movements: If the cancer has spread to the rectum, it can cause constipation or difficulty passing stool.
- Vaginal mass or lump: In some cases, a growth or mass may be felt in the vagina during pelvic exams.
- Back pain: Advanced vaginal cancer can cause lower back pain if it spreads to the lymph nodes or other areas.
- Swollen legs: Swelling in one or both legs can occur if the cancer blocks the lymphatic vessels.
It’s important to note that these symptoms can also be caused by other conditions, such as infections, cysts, or benign growths. However, if you experience any persistent or recurrent vaginal bleeding, discharge, or pelvic pain, it’s essential to consult your healthcare provider for proper evaluation and diagnosis.
Early detection and prompt treatment are crucial for improving the chances of successful management of vaginal cancer. Regular gynecological check-ups and awareness of any unusual symptoms can help catch the disease in its early stages when it is most treatable.
What are the causes of vaginal cancer?
Vaginal cancer is a rare type of cancer, and there are several potential causes and risk factors associated with its development. The main causes and risk factors for vaginal cancer include:
- Human papillomavirus (HPV) infection: Certain strains of HPV, particularly HPV-16 and HPV-18, are strongly linked to the development of vaginal cancer. HPV infections account for about 75% of vaginal cancers.
- Previous cervical cancer or pre-cancer: Women who have had cervical cancer or cervical pre-cancerous lesions (dysplasia) have an increased risk of developing vaginal cancer, as the cancerous cells can spread to the vagina.
- Exposure to diethylstilbestrol (DES): DES is a synthetic form of estrogen that was prescribed to pregnant women between 1940 and 1971 to prevent miscarriage. Daughters of women who took DES during pregnancy have a higher risk of developing a rare form of vaginal cancer called clear cell adenocarcinoma.
- Age: Vaginal cancer is more common in older women, typically those over the age of 60.
- Smoking: Long-term smoking has been associated with an increased risk of vaginal cancer, as well as other gynecological cancers.
- Immunosuppression: Women with weakened immune systems, such as those with HIV/AIDS or undergoing organ transplantation, have a higher risk of developing vaginal cancer due to their increased susceptibility to HPV infections.
- Previous radiation therapy: Radiation therapy to the pelvic area for the treatment of other cancers can increase the risk of developing vaginal cancer.
- Vaginal intraepithelial neoplasia (VAIN): VAIN is a pre-cancerous condition of the vaginal lining that can progress to vaginal cancer if left untreated.
It’s important to note that having one or more risk factors does not necessarily mean a woman will develop vaginal cancer. Regular gynecological check-ups, including Pap tests and HPV testing, can help detect precancerous changes and allow for early intervention and treatment.
What is the treatment for vaginal cancer?
The treatment for vaginal cancer depends on several factors, including the stage and type of cancer, the patient’s age and overall health, and their personal preferences. The main treatment options for vaginal cancer include:
- Surgery:
- For early-stage vaginal cancer, surgery is often the primary treatment. This may involve removing the affected part of the vagina (vaginectomy) or the entire vagina (radical vaginectomy).
- In some cases, a hysterectomy (removal of the uterus) and removal of nearby lymph nodes may also be performed.
- Radiation therapy:
- External beam radiation therapy uses high-energy X-rays or protons to kill cancer cells.
- Brachytherapy (internal radiation) involves placing radioactive sources directly inside or near the tumor.
- Radiation therapy may be used alone or in combination with surgery or chemotherapy.
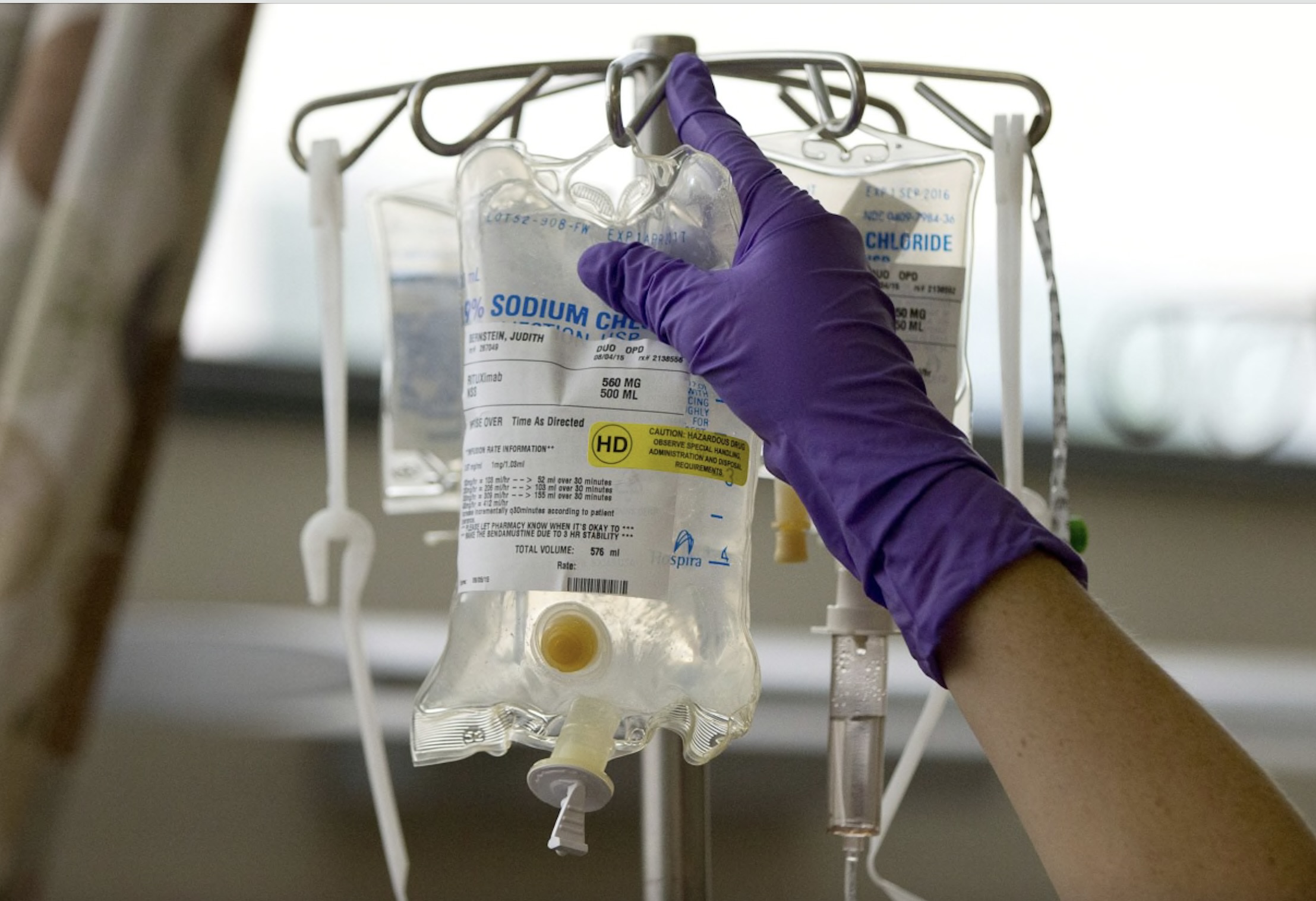
- Chemotherapy:
- Chemotherapy drugs are used to kill cancer cells and may be given intravenously or as a cream applied directly to the vagina.
- Chemotherapy is often combined with radiation therapy (chemoradiation) for more advanced stages of vaginal cancer.
- Topical therapy:
- For precancerous conditions or very early-stage vaginal cancer, topical chemotherapy or laser therapy may be used to remove or destroy the abnormal cells.
- Immunotherapy:
- Newer targeted therapies and immunotherapies, such as checkpoint inhibitors, may be an option for some patients with advanced or recurrent vaginal cancer.
The treatment plan is individualized based on the patient’s specific case and may involve a combination of these approaches. For example, surgery may be followed by radiation therapy or chemoradiation to reduce the risk of recurrence.
It’s important to discuss the potential benefits, risks, and side effects of each treatment option with a gynecologic oncologist or a multidisciplinary team of cancer specialists. Regular follow-up care and surveillance are also essential after treatment to monitor for any signs of recurrence or complications.