Ventricular Septal Defects: Symptoms, Causes, Treatment
What are the symptoms of a ventricular septal defect?
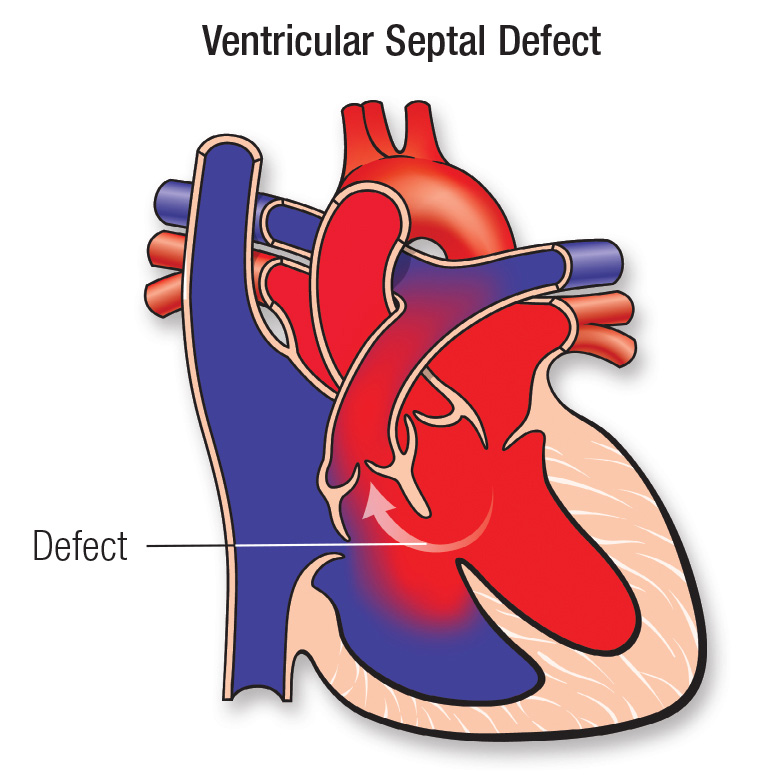
A ventricular septal defect (VSD) is a congenital heart defect where there is an abnormal opening in the wall (septum) between the two lower chambers (ventricles) of the heart. The symptoms of a VSD can vary depending on the size of the defect and other factors, but common symptoms may include:
- Heart murmur: A VSD often causes a heart murmur, which is an abnormal sound heard during a heartbeat. The murmur is caused by the flow of blood through the abnormal opening in the septum.
- Shortness of breath: In infants, rapid breathing or shortness of breath, especially during feeding, may be a symptom of a VSD.
- Poor feeding and failure to thrive: Infants with a VSD may have difficulty feeding and may not gain weight at a normal rate.
- Fatigue or weakness: Children or adults with a VSD may experience fatigue or weakness, especially during physical activity.
- Rapid heartbeat: A rapid or irregular heartbeat (arrhythmia) may occur in some cases of VSD.
- Frequent respiratory infections: Children with a VSD may be more prone to respiratory infections, such as pneumonia or bronchitis.
- Cyanosis: In severe cases of VSD, where there is significant mixing of oxygen-rich and oxygen-poor blood, cyanosis (a bluish tint to the skin, lips, or fingernails) may occur.
It’s important to note that not all individuals with a VSD will have symptoms, especially if the defect is small. Some VSDs may close on their own or may not cause significant problems. However, larger VSDs or those causing symptoms may require treatment, which may include medications or surgery to repair the defect. If you or your child is experiencing any symptoms of a VSD, it’s important to see a healthcare provider for an accurate diagnosis and appropriate management.
What are the causes of a ventricular septal defect?
A ventricular septal defect (VSD) is a congenital heart defect, meaning it is present at birth. The exact cause of VSDs is often unknown, but they are thought to occur during fetal development when the septum (wall) between the two lower chambers (ventricles) of the heart fails to fully form. Several factors may contribute to the development of VSDs, including:
- Genetic factors: VSDs can run in families, and certain genetic conditions, such as Down syndrome, are associated with an increased risk of VSDs.
- Maternal factors: Certain maternal factors, such as maternal diabetes, alcohol use, or certain medications taken during pregnancy, may increase the risk of VSDs in the fetus.
- Environmental factors: Exposure to certain environmental factors, such as chemicals or toxins, during pregnancy may increase the risk of VSDs.
- Chromosomal abnormalities: Certain chromosomal abnormalities, such as trisomy 13 or trisomy 18, are associated with an increased risk of VSDs.
- Other congenital heart defects: VSDs may occur in conjunction with other congenital heart defects, such as atrial septal defects (ASDs) or tetralogy of Fallot.
In many cases, the exact cause of a VSD is not identified. Most VSDs are diagnosed early in life, often during infancy, due to the presence of symptoms such as a heart murmur or cyanosis (bluish tint to the skin). Treatment for VSDs depends on the size and location of the defect, as well as the presence of symptoms. Small VSDs may close on their own without treatment, while larger VSDs or those causing symptoms may require medications or surgery to repair the defect.
What is the treatment for a ventricular septal defect?
The treatment for a ventricular septal defect (VSD) depends on several factors, including the size and location of the defect, the presence of symptoms, and the overall health of the patient. Treatment options for VSDs may include:
- Observation: Small VSDs that are not causing symptoms may be monitored over time without immediate treatment, as they may close on their own as the child grows.
- Medications: Medications may be used to manage symptoms and reduce the workload on the heart. These may include diuretics to reduce fluid buildup, medications to help the heart pump more effectively, or medications to control arrhythmias (irregular heartbeats).
- Surgery: In cases where the VSD is large or causing significant symptoms, surgery may be recommended to repair the defect. The most common surgical approach is open-heart surgery, during which the surgeon patches the hole in the septum using a synthetic patch or the patient’s own tissue.
- Catheter-based procedures: In some cases, especially for small to moderate-sized VSDs, a catheter-based procedure known as transcatheter closure may be used to close the defect. This procedure involves threading a catheter through a blood vessel to the heart, where a device is used to seal the hole in the septum.
- Lifestyle modifications: In some cases, lifestyle modifications such as regular exercise, a heart-healthy diet, and avoiding smoking or exposure to secondhand smoke may be recommended to help manage VSDs.
The specific treatment plan for a VSD will depend on the individual case and should be determined by a healthcare provider, typically a pediatric cardiologist or pediatric cardiac surgeon, with expertise in treating congenital heart defects. Regular follow-up care is important for monitoring the VSD and ensuring that any treatment is effective.