Ventricular Tachycardia: Symptoms, Causes, Treatment
What are the symptoms of ventricular tachycardia?
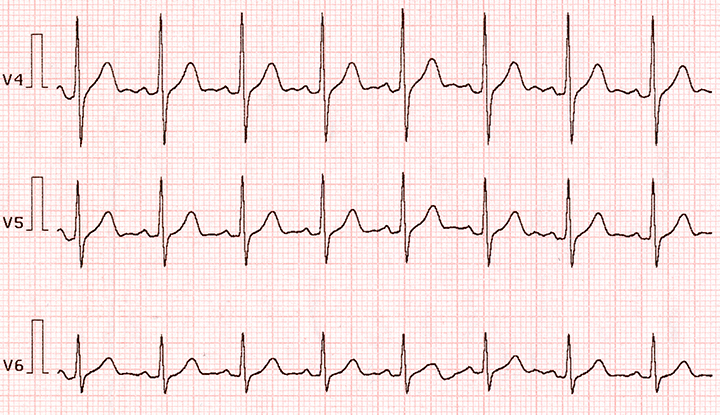
Ventricular tachycardia (VT) is a rapid heartbeat that originates in the lower chambers (ventricles) of the heart. It is characterized by a heart rate of more than 100 beats per minute, with three or more irregular heartbeats in a row. VT can be life-threatening and requires immediate medical attention. Symptoms of ventricular tachycardia may include:
- Palpitations: A sensation of rapid, fluttering, or pounding heartbeat.
- Dizziness or lightheadedness: Feeling faint or dizzy may occur, especially if the VT is causing a drop in blood pressure.
- Chest pain: Some people with VT may experience chest discomfort or pain.
- Shortness of breath: Difficulty breathing or feeling breathless, especially during physical activity or exertion.
- Fatigue: Feeling tired or lacking energy may occur, especially if the VT is prolonged or frequent.
- Fainting (syncope): In some cases, VT can cause fainting or loss of consciousness due to a lack of blood flow to the brain.
It’s important to note that some people with VT may not experience any symptoms, especially if the episodes are brief or infrequent. However, VT can be serious and may lead to more severe arrhythmias or cardiac arrest if not treated promptly. If you experience any symptoms of ventricular tachycardia, it’s important to seek immediate medical attention.
What are the causes of ventricular tachycardia?
Ventricular tachycardia (VT) can be caused by a variety of underlying heart conditions or other factors that affect the electrical system of the heart. Some common causes of ventricular tachycardia include:
- Coronary artery disease (CAD): Blockages in the coronary arteries can lead to decreased blood flow to the heart muscle, increasing the risk of VT.
- Cardiomyopathy: Diseases of the heart muscle, such as dilated cardiomyopathy or hypertrophic cardiomyopathy, can disrupt the heart’s electrical system and lead to VT.
- Myocardial infarction (heart attack): A heart attack can cause scar tissue to form in the heart, which can disrupt the heart’s normal electrical signals and lead to VT.
- Heart failure: Heart failure can lead to changes in the heart’s structure and function, increasing the risk of VT.
- Valvular heart disease: Conditions such as mitral valve prolapse or aortic stenosis can affect the heart’s electrical system and lead to VT.
- Congenital heart defects: Some people are born with structural abnormalities in their heart that can increase the risk of VT.
- Electrolyte imbalances: Imbalances in electrolytes such as potassium, sodium, or calcium can disrupt the heart’s electrical system and lead to VT.
- Certain medications: Some medications, such as antiarrhythmic drugs, can increase the risk of VT.
- Stimulants: Use of stimulants such as caffeine, nicotine, or certain illicit drugs can trigger VT in some people.
- Other factors: Other factors that can increase the risk of VT include age, gender (men are more likely to develop VT), and a family history of arrhythmias.
It’s important to note that ventricular tachycardia can be a serious condition that requires prompt medical evaluation and treatment. The underlying cause of VT should be determined by a healthcare provider, typically a cardiologist, who can recommend appropriate treatment based on the individual case.
What is the treatment for ventricular tachycardia?
The treatment for ventricular tachycardia (VT) depends on several factors, including the underlying cause of the arrhythmia, the severity of symptoms, and the risk of complications. Treatment options for VT may include:
- Antiarrhythmic medications: Medications such as amiodarone, lidocaine, or procainamide may be used to help control the heart rate and rhythm in people with VT.
- Cardioversion: In some cases, a procedure called cardioversion may be used to restore a normal heart rhythm. This can be done using medications or by delivering an electrical shock to the heart.
- Implantable cardioverter-defibrillator (ICD): An ICD is a device that is implanted under the skin and connected to the heart. It can detect and treat abnormal heart rhythms, including VT, by delivering a shock to restore a normal rhythm.
- Catheter ablation: In this procedure, a catheter is inserted into the heart and used to destroy (ablate) the tissue that is causing the abnormal electrical signals responsible for VT.
- Lifestyle changes: Making lifestyle changes such as quitting smoking, limiting alcohol and caffeine intake, and managing stress can help reduce the risk of VT.
- Treatment of underlying conditions: Treating underlying conditions such as coronary artery disease, cardiomyopathy, or electrolyte imbalances can help reduce the risk of VT.
- Emergency treatment: In cases where VT is causing severe symptoms or is not responding to other treatments, emergency treatments such as electrical cardioversion or medications to stabilize the heart rate and rhythm may be necessary.
It’s important for people with VT to work closely with a healthcare provider, typically a cardiologist or electrophysiologist, to develop an individualized treatment plan. Regular follow-up care is important to monitor the condition and adjust treatment as needed.