Achalasia: Symptoms, Causes, Treatment
What are the symptoms of achalasia?
Achalasia is a rare disorder that affects the esophagus, the muscular tube that carries food from the mouth to the stomach. The main symptoms of achalasia include:
- Difficulty swallowing (dysphagia): This is the most common symptom of achalasia. People with achalasia often have difficulty swallowing both solids and liquids, and food may get stuck in the esophagus.
- Regurgitation of food: Food that is not properly swallowed may come back up into the throat or mouth, especially when lying down or bending over.
- Chest pain: Some people with achalasia experience chest pain, which may be a burning or pressure-like sensation.
- Heartburn: Heartburn, or a burning sensation in the chest, may occur due to the backup of food and stomach acid into the esophagus.
- Weight loss: Difficulty swallowing and regurgitation can lead to weight loss and malnutrition.
- Coughing or choking: Some people with achalasia may experience coughing or choking, especially while eating or drinking.
- Difficulty belching: Belching, or burping, may be difficult or impossible for people with achalasia due to the inability of the esophageal sphincter to relax.
- Bad breath: Regurgitated food and stomach acid can lead to bad breath (halitosis).
Symptoms of achalasia can vary in severity and may come and go over time. If you experience persistent difficulty swallowing or other symptoms of achalasia, it’s important to see a healthcare provider for proper evaluation and diagnosis.
What are the causes of achalasia?
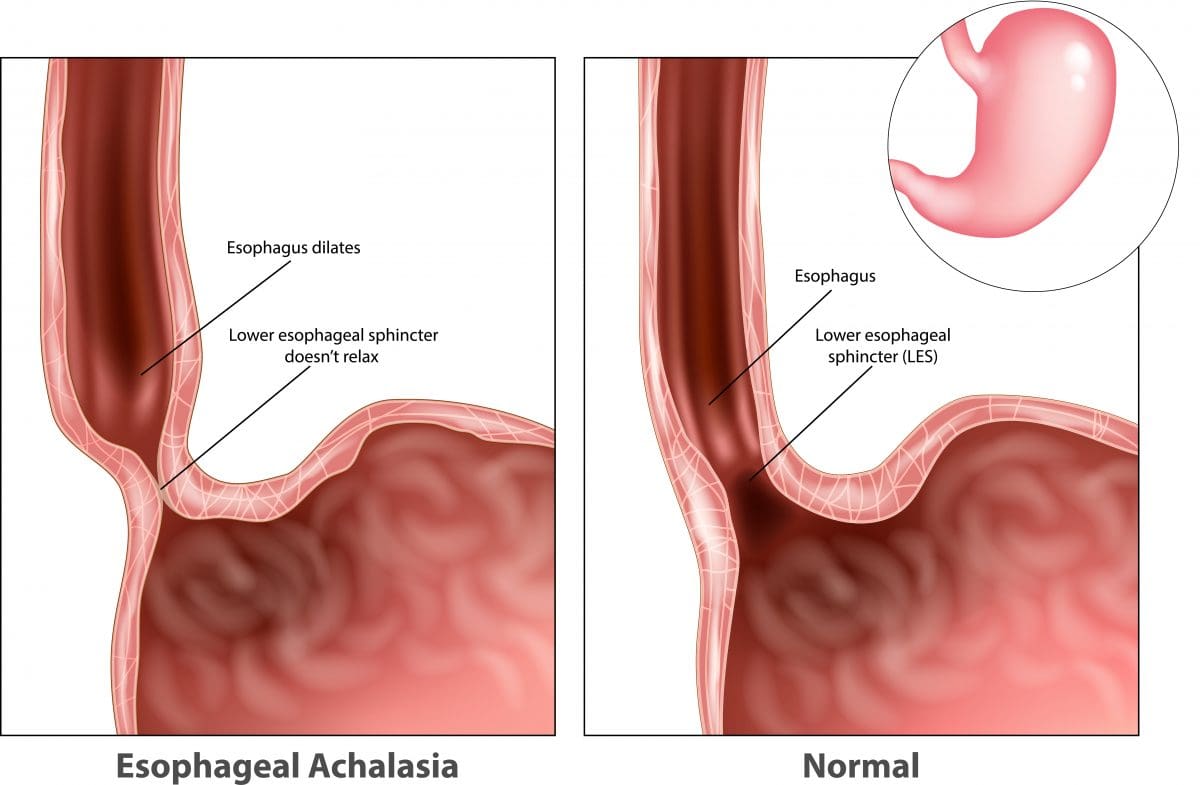
Achalasia is believed to be caused by damage to the nerves in the esophagus, specifically the nerves that control the muscles that normally push food down the esophagus and into the stomach (peristalsis), as well as the lower esophageal sphincter (LES), which is the muscular ring that normally relaxes to allow food to pass into the stomach.
The exact cause of this nerve damage is not well understood, but several factors may contribute to the development of achalasia:
- Autoimmune reaction: Some researchers believe that achalasia may be an autoimmune disorder, where the body’s immune system mistakenly attacks the nerves in the esophagus.
- Infection: Certain viral infections, such as herpes simplex virus, have been proposed as possible triggers for the autoimmune reaction that leads to nerve damage in achalasia.
- Genetics: There may be a genetic predisposition to developing achalasia, as the condition sometimes runs in families.
- Other factors: Other factors, such as abnormalities in the esophageal muscles or the LES, may contribute to the development of achalasia, but these are less well understood.
It’s important to note that while these factors may play a role in the development of achalasia, the exact cause is not always clear, and more research is needed to fully understand the condition. Achalasia is a rare disorder, and most cases occur sporadically without a clear cause.
What is the treatment for achalasia?
Treatment for achalasia is aimed at relieving symptoms and improving esophageal function. The choice of treatment depends on the severity of symptoms and the individual’s overall health. Treatment options may include:
- Balloon dilation (pneumatic dilation): This is a procedure where a balloon is inserted into the esophagus and inflated to stretch the lower esophageal sphincter (LES), allowing food to pass more easily into the stomach. Balloon dilation is often effective in improving swallowing and relieving symptoms, but the effects may not be permanent, and the procedure may need to be repeated. I had balloon dilation done on me a dozen or so times, and it caused a hernia. I stopped doing the dilations and have been doing fine for the most part.
- Botulinum toxin (Botox) injection: In this procedure, botulinum toxin is injected into the LES to relax the muscle and improve swallowing. This treatment is less invasive than balloon dilation but may need to be repeated every few months.
- Surgery (myotomy): In some cases, surgery may be recommended to cut the muscles of the LES, allowing food to pass more easily into the stomach. This procedure is usually done laparoscopically (minimally invasive surgery) and is effective in relieving symptoms in most cases.
- Medications: Medications such as calcium channel blockers or nitrates may be prescribed to help relax the LES and improve swallowing, but they are usually less effective than other treatments and may have side effects.
- Lifestyle changes: Making changes to your eating habits, such as eating smaller, more frequent meals and avoiding foods that trigger symptoms, can help manage achalasia symptoms.
- Endoscopic therapy: In some cases, endoscopic therapies such as per-oral endoscopic myotomy (POEM) or endoscopic balloon dilation may be used to treat achalasia. These procedures are less invasive than surgery but may not be suitable for all patients.
The choice of treatment depends on various factors, including the severity of symptoms, the presence of complications, and the individual’s overall health and preferences. It’s important to discuss treatment options with a healthcare provider to determine the most appropriate approach for managing achalasia.
TL;DR: What is Achalasia?
Achalasia is a rare disorder that affects the esophagus, which is the muscular tube that carries food and liquids from the mouth to the stomach.
In achalasia, the lower esophageal sphincter (LES), a ring-like muscle at the bottom of the esophagus, fails to relax properly when swallowing. This leads to difficulty in pushing food down into the stomach. Additionally, the esophagus loses its ability to contract and move food down through peristalsis.
Here are some key points about achalasia:
- Causes: The exact cause of achalasia is unknown, but it is believed to be related to the degeneration of the nerve cells that control the relaxation and contraction of the esophageal muscles. It is not inherited and is not caused by any known external factors.
- Symptoms: The main symptom of achalasia is difficulty swallowing (dysphagia), particularly with solid foods. Other symptoms may include regurgitation of undigested food, chest pain, weight loss, and a feeling of fullness or discomfort in the chest or throat.
- Diagnosis: Achalasia is typically diagnosed through a combination of tests, including:
- Barium swallow or esophagogram (an X-ray of the esophagus after swallowing a barium solution)
- Endoscopy (insertion of a flexible tube with a camera to examine the esophagus)
- Esophageal manometry (measuring the pressure and contractions of the esophagus)
- Treatment: While there is no cure for achalasia, various treatments can help manage the symptoms and improve swallowing function:
- Oral medications (nitrates or calcium channel blockers) to relax the LES
- Botulinum toxin (Botox) injections into the LES to relax the muscle temporarily
- Pneumatic dilation (stretching the LES with an inflatable balloon)
- Surgical myotomy (cutting the LES muscle to allow food to pass through)
- Esophagectomy (surgical removal of the esophagus) in severe, advanced cases
- Complications: Untreated achalasia can lead to complications such as weight loss, malnutrition, aspiration pneumonia (from regurgitated food entering the lungs), and esophageal dilation or widening.
Achalasia is a chronic condition that requires ongoing management and monitoring. Early diagnosis and appropriate treatment can help improve swallowing function, prevent complications, and maintain adequate nutrition and quality of life for individuals with this condition.