What Is an Oophorectomy?
An oophorectomy is a surgical procedure to remove one or both of the ovaries. The ovaries are the female reproductive organs that produce eggs and hormones such as estrogen and progesterone. An oophorectomy may be performed as part of a treatment plan for conditions such as ovarian cancer, endometriosis, ovarian torsion, or certain types of ovarian cysts. It may also be performed as a preventive measure in women at high risk for ovarian cancer or as part of gender-affirming surgery for transgender individuals.
What are the reasons for oophorectomy?
There are several reasons why an oophorectomy may be performed:
- Ovarian Cancer: Oophorectomy may be recommended as part of the treatment for ovarian cancer, especially if the cancer is confined to the ovaries or if there is a high risk of the cancer returning.
- Endometriosis: In cases of severe endometriosis that do not respond to other treatments, oophorectomy may be considered to remove the ovaries, which are a source of estrogen that can stimulate endometrial growth.
- Ovarian Torsion: Oophorectomy may be necessary in cases of ovarian torsion, which is a condition where the ovary twists on its blood supply, cutting off blood flow to the ovary.
- Ovarian Cysts: Large or persistent ovarian cysts that are causing symptoms or are at risk of rupture may require oophorectomy.
- High Risk of Ovarian Cancer: Women with a strong family history of ovarian cancer or certain genetic mutations (such as BRCA1 or BRCA2) that increase the risk of ovarian cancer may choose to undergo oophorectomy as a preventive measure.
- Gender-Affirming Surgery: Oophorectomy may be performed as part of gender-affirming surgery for transgender individuals as part of the process of transitioning.
- Pelvic Inflammatory Disease (PID): In severe cases of PID that have caused significant damage to the ovaries, oophorectomy may be necessary.
- Chronic Pelvic Pain: In some cases of chronic pelvic pain that is not responsive to other treatments, oophorectomy may be considered as a last resort.
The decision to undergo oophorectomy is based on the individual’s specific condition, overall health, and personal preferences. It is important to discuss the risks and benefits of the procedure with a healthcare provider before making a decision.
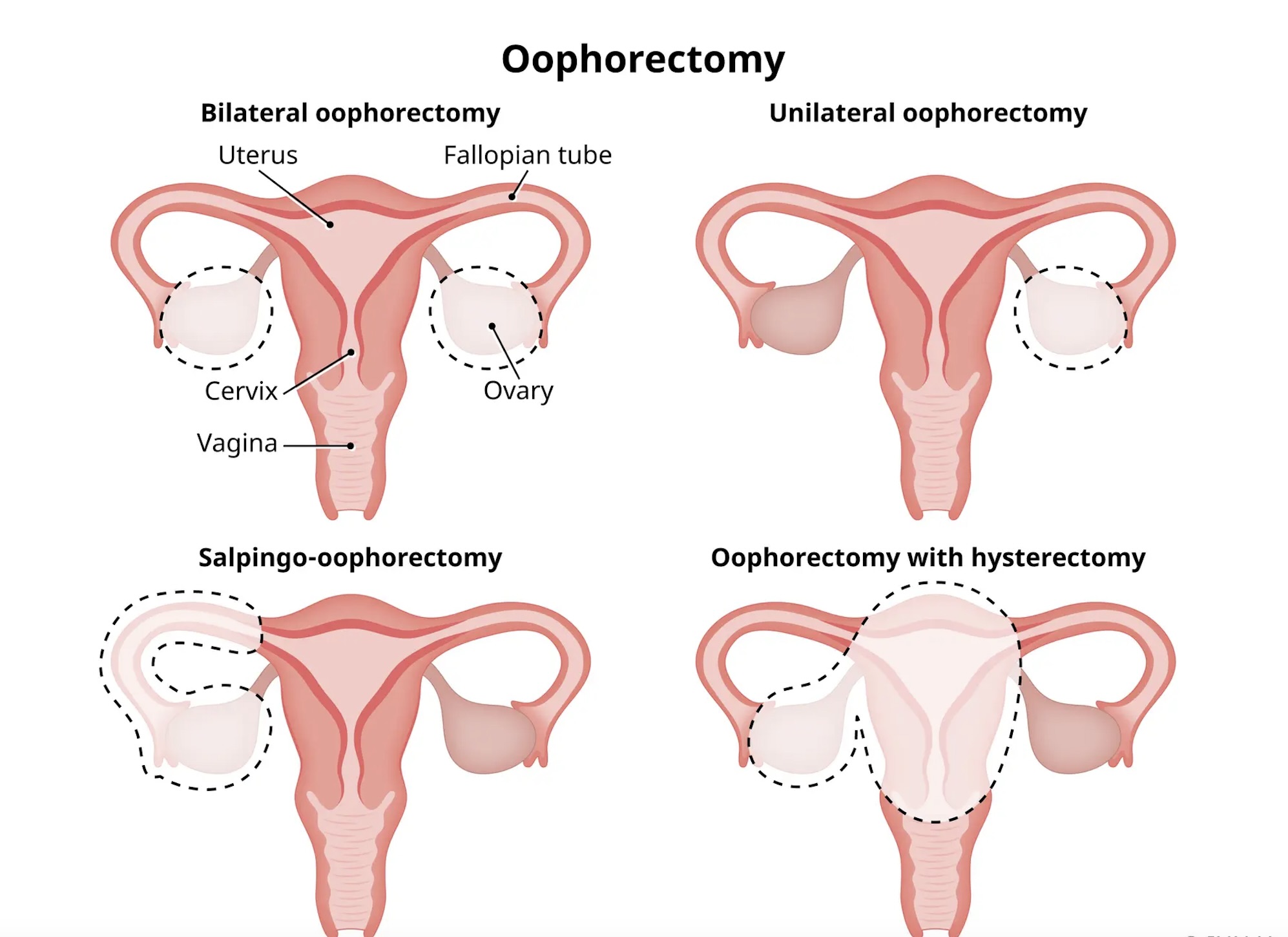
What are the types of oophorectomy?
There are two main types of oophorectomy:
- Unilateral Oophorectomy: In this procedure, only one ovary is removed. It is often performed when there is a cyst, tumor, or other condition affecting one ovary, while the other ovary remains healthy.
- Bilateral Oophorectomy: In this procedure, both ovaries are removed. It may be performed for various reasons, including cancer treatment, prevention of ovarian cancer in high-risk individuals, or as part of gender-affirming surgery for transgender individuals.
Both unilateral and bilateral oophorectomies can be performed using different surgical approaches, including:
- Laparoscopic Oophorectomy: A minimally invasive procedure in which small incisions are made in the abdomen, and a laparoscope (a thin, flexible tube with a camera) is used to guide the surgery. This approach typically results in less pain and a quicker recovery compared to traditional open surgery.
- Robotic-Assisted Oophorectomy: Similar to laparoscopic oophorectomy, but the surgeon uses a robotic system to control the surgical instruments. This approach can provide enhanced precision and dexterity.
- Open Oophorectomy: A traditional surgical approach in which a larger incision is made in the abdomen to access the ovaries. This approach may be necessary for complex cases or when the surgeon needs better access to the ovaries.
The choice of surgical approach depends on the specific circumstances of the patient’s condition, the surgeon’s expertise, and other factors. It’s important to discuss the options with a healthcare provider to determine the most appropriate approach for each individual case.
What are the risks associated with oophorectomy?
Oophorectomy, like any surgical procedure, carries certain risks. Some potential risks and complications associated with oophorectomy include:
- Infection: There is a risk of developing an infection at the surgical site or in the pelvic area.
- Bleeding: Excessive bleeding during or after surgery is a potential risk, especially in cases of large or deep-seated tumors.
- Blood Clots: Surgery increases the risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism).
- Damage to Surrounding Organs: There is a small risk of accidental damage to nearby organs, such as the bladder or intestines, during surgery.
- Adverse Reaction to Anesthesia: Some individuals may experience an allergic reaction or other complications related to anesthesia.
- Menopausal Symptoms: If both ovaries are removed, the sudden decrease in estrogen levels can lead to menopausal symptoms such as hot flashes, vaginal dryness, and mood changes.
- Bone Health: Removal of the ovaries can increase the risk of osteoporosis (weakening of the bones) due to the decrease in estrogen levels.
- Cardiovascular Health: Early menopause resulting from oophorectomy may increase the risk of cardiovascular disease.
- Sexual Function: Oophorectomy can affect sexual function, including decreased libido and vaginal dryness, especially if both ovaries are removed.
- Psychological Impact: Some individuals may experience emotional distress or psychological effects related to the removal of the ovaries.
It’s important to discuss these risks with your healthcare provider before undergoing oophorectomy. In some cases, the benefits of the procedure may outweigh the risks, especially in cases of cancer treatment or prevention. However, the decision to undergo oophorectomy should be based on a thorough evaluation of your individual circumstances and preferences.